Modern Patient Room Design with Peter O’Connor from Inova
Digital Health Frontiers – Podcast Ep. 3

IT Director, Eastern Region & IT Solutions Design Group, Inova

President and COO
Caregility
In this episode of the Digital Health Frontiers, Caregility President and COO Mike Brandofino sits down with Peter O’Connor, Director of IT for Inova’s Eastern Region Development Program, to discuss the health system’s approach to modern patient room design. Drawing from over 30 years of experience in healthcare technology design and facility architecture, Peter shares insights into Inova’s highly collaborative approach to clinical IT enablement, which seeks to elevate patient and staff experience through hybrid care models that integrate telehealth and other technologies into bedside care.
Mike and Peter explore the integration of technology in patient care delivery, the unique task of bridging gaps between design, construction, and clinical processes, and the innovative virtual care programs that are transforming bedside care at Inova. Peter highlights the importance of culture, leadership support, and strong partnerships in driving these initiatives forward. Tune in to learn how Inova is setting new standards in healthcare delivery using technology to create seamless, patient-first experiences.
Read the Transcript
Welcome to Digital Health Frontiers, where we explore the cutting edge of healthcare technology, policy, and innovation, hosted by Mike Brandofino, President and COO of Caregility. Today Mike is joined by Peter O’Connor, the Director of IT for Inova’s Eastern Region Development Program which includes two new state-of-the-art hospital campuses totaling over 1.5 million square feet, as well as a new ambulatory facility that will include a full-service emergency room, ambulatory surgery, imaging services, a family medicine center and medical offices. Peter leverages his 33 years of technology design, implementation, and consulting experience to ensure that clinical process is enabled by technologies that meet the immediate clinical need, fit within Inova’s clinical IT ecosystem, and support the health system’s long-term digital strategy. Today Peter joins Mike to share insight into his approach to patient room design at Inova.
Mike Brandofino:
Hello everybody. Today with me, I have Peter O’Connor from Inova to talk about some of the experiences that they’ve had implementing virtual care within their health system. Hey Peter. Thank you very much for joining.
Peter O’Connor:
It’s my pleasure, Mike. Thanks for having me.
Brandofino:
Can you just describe the health system for the audience, so they get a little idea of what you guys are up to?
O’Connor:
Sure. Inova is Northern Virginia’s leading not-for-profit healthcare provider. So our mission is to provide world-class healthcare every time, every touch, to every person in every community that we have the privilege to serve. We’ve got about 20,000 team members that provide more than two million patient visits a year. We have an integrated network of five hospitals, approximately 2,000 beds, and lots of primary and specialty care practices. And interestingly enough, we’re the fourth busiest emergency room in the nation, so our hospitals are recognized with the US News and world reports. In fact, our Fairfax Hospital is the number one hospital in the DC metro area. We’re in the top 50 in neonatology, and top 20 in the nation for OBGYN.
Brandofino:
So, can you talk a little bit about your role? I think it’s a little unique, although I think some health systems are starting to put some focus around this. But can you talk a little about your focus and your position?
O’Connor:
Sure. It’s been really fantastic and it’s been a role that I really feel like my career – which is going on 33 years – I feel like the last 30 years have really prepared me for. We have a unique team at Inova for design and construction. I’d say we have a bit of a dream team. We’ve got our own engineers, architects, former contractors, & Clinical and operation experts. So, in my almost now 40 years I’ve never seen in healthcare design and construction an owner’s team with this level of experience.
So my role is pretty interesting. I bridge the gap between design and construction, IT, clinical engineering, and operations, which are typically siloed in a design process. The Inova leadership team saw an opportunity to have somebody with experience in all of those bridge the gaps and translate clinical process and what it’s going to look like in 2028 into enabling technologies and then turn that into something that can be procured and also built.
Brandofino:
You know, it’s such an interesting role and I wish more health systems would have that. So many times we’ll be talking just to the clinical side and then then when you start talking about implementing any kind of solution then either the technical side or even the facility side comes in and goes “oh, no, no -you can’t do that because of this,” or “hey, did you know there’s a lead plate in the wall next to the room that you wanted to do that Wi-Fi in?” So, I think it’s really an interesting role.
What’s it like to bridge that gap and pull those people into the same room, so to speak?
O’Connor:
It’s honestly exciting. It’s knowing that we can pull those people together in a collaborative space and brainstorm and learn from each other and really feed off of each other’s energy. It’s one of the reasons I came to Inova. I’ve had the privilege of working with lots of hospitals throughout my career in the architecture and engineering world and I’ve found that a lot of — if you could imagine folks swimming in a pool — that a lot of times it’s exactly what you said. Biomed may be going one direction, clinicians may be going in another, IT may be going another, and everyone’s swimming in a different direction. At Inova, I found that everybody was swimming in the same direction and with the same objectives and my role allows me to lift those little buoys in between the swim lanes and have everybody kind of work together and go in that same direction and see what other people are doing and leverage those experiences and come up with some really innovative solutions.
Brandofino:
How much does the patient experience fit into what you guys are trying to do?
O’Connor:
Patient experience is obviously essential. From my perspective, from a technology perspective, we want that technology to be seamless, and transparent, and to always enhance the patient and caregiver experience. When that technology becomes front-of-mind, kind of replacing healing and care front-of-mind, we’ve done something wrong. We have a tremendous responsibility to design places that heal, places that – on somebody’s worst day, whenever they feel they’ve lost all control over their environment – use technology as one of those ways to help them find some level of control and normalcy through access to information, access to education, control over their environment, access to the amazing bedside team, and make that as simple as possible for the patient. That patient experience and bringing some level of normalcy and control to a very hectic time in their world is critical for us.
Brandofino:
We spend so much time focusing, even as Caregility, on the clinician, primarily the nurse because they’re the ones using the technology the most, but we can’t forget the patient experience and what they’re going through. So that’s great that you guys have focus on that.
O’Connor:
Our IT and nursing leadership consistently remind all 650 of us IT teammates that were part of the care team. They encourage our IT team, whether you’re in leadership or you’re an analyst or you’re in the service side, to round just like the clinicians do. So, spending time on those various units gives you that real perspective of the patient and the teammate experience. Simply put, our mission is to get the right information to the right people at the right time to make great decisions.
Brandofino:
Sure. Well, stay on the clinical team. We have we have a chief nursing officer and some nurses on staff and I constantly get, “But Mike, you don’t understand what the nurse is going through in the room at the time. You’ve got to consider that.”
What insights are you getting from your clinical team as it relates to helping them in the day-in-the-life of a caregiver?
O’Connor:
We’ve had this pretty extensive design process for our new Eastern region expansion, which is two full size hospitals, full medical campuses, a Cancer Center, a specialty care center, about a million and a half square feet. So over the last two years, we’ve had thousands of hours of clinical input. We even built full-scale mock-ups of patient rooms, treatment rooms, ORs, imaging spaces, even the team stations to ensure that those designs work within that clinical workflow.
But, also, they were prepared for future technology and clinical processes. So having the clinical team come into, let’s say, a hybrid OR and they can move all the pieces around and they can mock a code or they can mock a certain procedure – gives us insight that you can’t get out of looking at a floor plan, or even can’t really get out of some of the 3D modeling. It’s just nothing beats walking into a room that’s fully constructed, and they can move things around, which is fantastic.
I would say that one of the keys to our success has been that our projects are led by a clinical team. It’s a million and a half square foot Eastern Region Expansion led by a clinical team. Heather Russell is our VP of Eastern Region Development. Eric Miller is our director of Eastern Region Development. They both have extensive clinical backgrounds. They’ve been instrumental in ensuring that the clinical voice is not only heard, but also that the clinical process is understood by everybody involved – all of us internal experts, the design construction and architecture teams. So having a construction project led by clinical operations and supported by in-house industry experts has really been our secret to success and taking that clinical voice and translating it into something that can actually be built.
Brandofino:
That’s great. Having the buy-in it is going to help. What are your biggest challenges? Sometimes the challenge is just people having an aversion to change and others are just that some of these hospitals are old or challenging to change, especially with patients in rooms and it’s kind of like changing the chassis on the car while it’s moving.
What are some of your biggest challenges?
O’Connor:
I guess from a change perspective, you’re talking about physical change from an infrastructure, but also change from a culture and thought process perspective. The good news is our CEO, Dr. Steven Jones, reminds us all – and this is in all of our Web leadership meetings, in-person leadership meetings, any time that we’re fortunate to spend with him – he reminds us to challenge the status quo and always ask why. That spirit of unrestrained curiosity has led us to either reevaluate and reconfirm current processes or quite often, it’s been the catalyst for change and to explore the why-nots and make them real. So, from a culture perspective, we are well positioned to embrace change, look for change, ask for change from the clinical level through the IT level, and design, and construction, and facilities – you name it.
But some of the challenges that we have is taking all of that that we’ve envisioned for change and documenting it well. When you’re looking at a million and a half square feet of design and you’re trying to coordinate architecture, MEP, medical equipment and technologies, security, AV, there’s a lot of moving sites or moving parts for three sites that we’re building. Traditionally projects like this, the lack of decision or direction is usually the biggest challenge. Fortunately, with our clinical leadership team on the project that’s not been a challenge really. It’s making sure that all those voices and all those hours of work and working through the clinical processes and translating that into a built environment gets documented well and gets constructed the way we expect it.
Brandofino:
That’s great. It sounds like the executive team is close to these projects and provides you that aircover that you need. That’s great to see. We’re seeing some customers who lack that kind of centralized support. You have pockets of folks fighting to try and get the attention, the funding, and get their program projects through. It seems like you guys have kind of centralized that and have the executive team providing overall air cover.
O’Connor:
We do. Our executive team, our C-level team, knows about every square foot of the new construction. Heather, being a nurse herself and a senior member of our core leadership team, that visibility and that voice – anything that we need, decisions to be made, executive direction – it’s one phone call away with Heather. And from an IT perspective, our Chief Digital Information Officer and our Chief Technology Officer are highly engaged as well as all the senior members of our networking cybersecurity infrastructure team. So, from day one, everybody’s been engaged in these projects. Throughout my career – as I’ve mentioned, I’ve worked on other projects – I haven’t seen that level of engagement. As you said, I’ve seen pockets of engagement. I don’t think I’ve ever seen the systemwide level of investment of time, energy and, direction in projects like this.
Brandofino:
That’s great. In projects this scale and size, you have multiple vendors and partners – we like to consider ourselves a partner because we’re in this for the long haul with our customers.
What are you looking for in vendors and partners as these projects progress?
O’Connor:
The scale of what we’re doing – we’re adding a million and a half square feet, two new campuses, but we also have five existing campuses and 7,000 nurses and so you’ve got a very complex existing enterprise environment and then you’re adding on to it with new construction and innovation. How do you take some of that new technology and put it into the existing environment and how do you take ideas that we want to do today and translate that into something in 2028?
What we look for are industry segment leaders that want to collaborate. Folks that are innovative themselves. They’re looking to the future. We want partners to have that same “why or why not” conversation with us and that we can have with them. It is truly that partnership of collaboration. Folks that fit into the Inova culture, that have that mindset. We need partners that are willing to work with other partners and create enhanced integrations that enable that seamless experience that I identified earlier. Without that type of collaboration and partnership – and as you said, in for the long haul – it’s not going to be easy. We’re going to be pushing and pulling on each other. But I’m a firm believer that sometimes you go through a little heat, and you create relationships. The strongest bonds are formed with heat sometimes and so you get a great partner that will get in the trenches with you and help figure this out. And then everything just seems to work out for the best. So, we’re fortunate to have wonderful, wonderful partners.
Brandofino:
That’s great. So, the buzzword right now in healthcare is Virtual Nursing. Hybrid care is another term for it. We’re actually seeing some tremendous feedback. Customer satisfaction is up. Nurse retention is up because of it in some of our health systems.
How is your organization thinking about hybrid care? Is it being embraced and are you seeing any success at it yet if you’re actually going down that path?
O’Connor:
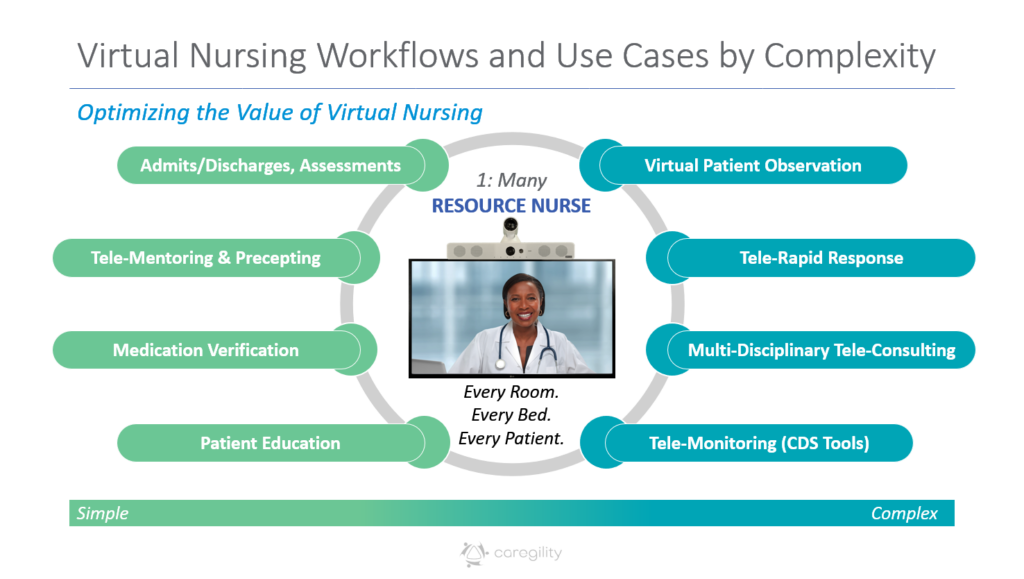
We’ve transitioned from thinking about virtual care to living it and breathing it every day. We’ve got some innovative thought leaders from our Chief Nursing Information Officer, Maggie, our Chief Health Information Officer, Dr. Kramer, and our Senior Director of Telemedicine, Steve. We have implemented an industry-leading Virtual Nurse program, which began with some basic use cases with virtual admit and discharge, patient education, patient pain reassessment. Those use cases alone have reduced bedside time by roughly 30 minutes per nurse per shift. So, you can imagine giving 30 minutes per nurse per shift back to that bedside nurse to do the things that he or she is really, you know, in their heart, they want to do. They want to deliver bedside care, right? Not be going through a lot of things, so it’s a great use to those resources and somebody that can step in virtually and assist that patient in whatever they may need.
So now, since that’s been so successful, we’re now looking to dual consent, we’re looking to case management and wound care as additional telemedicine applications or virtual care applications. So again, expanding that footprint, that technology that we’ve invested in. You guys have been a phenomenal partner with us in doing that. So just extending that program, so all of our five sites are connected back to what we consider a very innovative high-reliability Operations Center, which is our rock where Virtual Nursing, our Central Telemetry, our Central Sitting Resource Management, our Transfer Team all operate out of the same suite on one of our floors in our corporate campus. So, you can imagine all those folks are together to make great decisions about moving patients, taking care of patients, all in that same area. We’re looking at serving 2,000 beds out of a central location. It’s been pretty innovative and it’s been open almost a year now and we’ve had nothing but tremendous feedback from our nursing teams and our patients.
Brandofino:
That’s great. We love to hear that because I think we’re getting close to a time where you could just cross out “tele” and “virtual” and it is just healthcare. It’s the way we have to deliver healthcare these days. You mentioned in the partnership, the need to be able to work together.
So how important are integrations? And from that perspective, what do you think the vision is of patient experience in Inova as you go forward?
O’Connor:
I keep on coming back to that word “transparent.” Those integrations have to be what I consider invisibly critical. And today, you know, in our personal lives, we all expect context in our alerts and how we integrate with our devices and you know the ability to delineate the noise from what’s really important and the same goes for our healthcare environment. You know the EHR gives us context, the nurse call is that patient’s lifeline, the interactive patient engagement system is that medium to provide education and information, and virtual care is that reassurance that you have a multidisciplinary team ready and available to be there whenever our patients need them, whether it’s in the patient room setting or it’s in the emergency room or it’s at home.
To your point, I think it is just healthcare. It is just a different way to meet people where they are and I think so often healthcare institutions have this mindset of “you have to come to our site, you have to be in our room.” We have two million patients that we have the privilege to serve and finding the best way possible to do that in whatever environment it needs to be is really where we need to be as an industry.
Brandofino:
Something that’s been top of mind for a lot of folks — from an ROI perspective, there’s soft-dollar ROI, there’s hard-dollar ROI – how does your CFO look at some of this? Do they consider the soft-dollar ROI as well? That patient satisfaction, the nurse satisfaction. Does that play into your ability to continue to expand these programs?
O’Connor:
Oh, absolutely. So we’re always patient-first. Fortunately, we’re a very successful not-for-profit healthcare system, and our ability to reinvest in our infrastructure, reinvest in our people, reinvest in the community and programs, we’re very blessed to be able to do that. But in order to do that, we have to be operationally efficient. We have to have the volume of patients that people want to come to Inova and want to be treated at Inova. So it does come down to those soft dollars. They are really hard to put a number on or a value on, but, again, we’re patient first so having our care team enabled with the best technology, having them to do what they do best at the bedside, having the best diagnostics and ability to intervene and deliver care – it is the most important thing to us at the end of the day. If we’re successful financially doing that it just gives us the ability to do that even more in more places to more people and have better technology.
Being a not-for-profit, private healthcare institution is a really unique thing and we’re really in control of our destiny and how we apply those resources. Our leadership team has done a wonderful job with that balance of growth and reinvesting in our infrastructure and also caring for our communities and the people who are less fortunate who can’t afford care.
Brandofino:
Clearly, you guys are a leader, and your role alone. What to me is unique in the space is really taking this seriously and putting some resources around it that really understand how to move these projects forward.
So for those health systems that are watching this, that maybe haven’t gotten started yet or had some stop/starts, can you give them a nugget of advice that can help them on their way?
O’Connor:
I think for us it’s been creating a culture where people are open and willing to listen to what doesn’t work and have the courage to ask “why not.” Having executive leadership supporting change and having partners that can collaborate and not be afraid to add a couple of destinations on the road map for us is critical. I think that the key to our success, it really does come down to – at least for me – it’s culture. It’s having an environment that lets us explore and innovate without being so adherent to recorded direction. We’re always asked the question or encouraged to ask the question “why” so for me, it’s been a culture thing.
You would think that this is all tech and innovation and being able to try different things. If you’re not in an environment that supports that, all the technology in the world is not going to help you. So it’s having the culture. Change starts with the culture.
Brandofino:
You speak my language. I always have said technology for technology’s sake is just not the way to go. If you can get the buy-in, if you have that culture that is willing to try things and fail fast, right? Not everything is going to work the first time, but if you’re willing to fail fast and try new things, I think you end up accomplishing a lot more than those who kind of wait for that perfect thing, whatever it is.
O’Connor:
Absolutely. The ability to do pilot programs and having partners willing to help us out and see what works and what doesn’t work. In an environment where you’ve you’re confident and you’ve got the confidence in your leadership team that you can try and fail and then you get up and you try again and this works. Having that environment is fantastic. We have a lot of exciting things ahead of us and we look forward to building an infrastructure where we have virtual health in every patient room. All of our new construction, we’ve got it planned and we’re working on processes and plans to move that into existing care spaces today. So you just have to position yourself and look towards the future and the future is, to your point, just healthcare. It’s not virtual health, it’s not inpatient healthcare. It’s just healthcare.
Brandofino:
Well, Peter, thank you very much for taking the time to share your experience and your story with hopefully a lot of healthcare systems that will learn from this. I really appreciate it and thanks for joining.
O’Connor:
Thanks for having me. Have a wonderful day.
Subscribe to Digital Health Frontiers and listen in on your favorite podcast app here.