Baptist Health, Caregility Expand Partnership to Enhance Patient Care
Arkansas-based health system to more than double its bedside telehealth footprint with
expansion of virtual nursing, support staff, and providers
EATONTOWN, N.J. and LITTLE ROCK, Ark. (May 9, 2024) – Baptist Health and Caregility are pleased to announce an expanded partnership aimed at enhancing patient care across the Arkansas-based healthcare organization.
Baptist Health will enhance its bedside care teams by increasing its usage of Caregility intelligent telehealth devices to more than 700 bedsides system-wide, doubling the footprint of the healthcare organization’s inpatient telehealth services. The initiative adds virtual clinical resources to support in-person bedside care and help improve patient outcomes. This collaboration underscores both organizations’ commitment to leveraging technology to transform healthcare delivery and meet the evolving needs of patients and staff.
The enhanced partnership builds upon Baptist Health’s previous success with virtual admissions and discharge programs, currently supported by more than 300 wall-mounted and cart-based Caregility telehealth devices across 11 hospitals. Since partnering on virtual care services with Caregility in 2021, telehealth session volume for Baptist Health has increased from roughly 1,000 virtual visits per quarter to more than 20,000.

In early 2023, Baptist Health Rehabilitation Institute successfully launched Arkansas’ first virtual nursing program to provide additional support to bedside nurses, patients and families. The program then expanded to the healing ministry’s hospitals in Stuttgart, Malvern and Heber Springs. Thanks to positive patient outcomes and feedback, Baptist Health will roll out virtual care programs on every medical and surgical floor across the organization.
As part of this expansion, Baptist Health will deploy Caregility’s new, highly advanced telehealth devices and award-winning Caregility Cloud™ virtual care platform in more than 500 additional patient rooms at the health system’s flagship hospital, Baptist Health Medical Center-Little Rock, as well as Baptist Health Medical Center-North Little Rock and Baptist Health-Fort Smith. These devices will support the expansion of virtual nursing and the rollout of virtual support staff and virtual providers in the coming months. Additionally, a centralized hub to support virtual nursing and virtual sitters has opened on the Baptist Health Medical Center-Little Rock campus.

“Embracing virtual support as part of our acute care bedside support and quality strategy signifies a pivotal step forward in how we envision the future of healthcare at Baptist Health. Baptist Health first added virtual care in 2005, and we have continued to advance with the latest technology bringing us to where we are today with our partnership with Caregility. This expansion is more than an initiative; it’s a commitment to providing health equity across our state, setting new standards in patient and provider satisfaction, and furthering our mission to be the employer of choice in Arkansas.”
– Kourtney Matlock
President of Baptist Health Rehabilitation Institute
and system post-acute services
The partnership exponentially increases the eyes and ears able to focus on patients, reducing pressure on bedside staff by redistributing tasks that a virtual nurse or support staff can field. As a result of increased telehealth services in acute care settings, healthcare systems see significant time savings and improved throughput (the process of moving patients through the hospital system from admission to discharge). Having virtual options at the bedside appeals to patients as well, as evidenced by improved patient satisfaction ratings in early field trials.
“We are at a point where this type of care model is not an option for our health systems, it is the only way they can address staffing issues and remain competitive,” said Caregility President and COO Mike Brandofino. “This partnership with Baptist Health is a great example of how Caregility can make it easy to deploy intelligent devices and services to enhance patient care through virtual programs.”
Caregility Cloud™ allows health systems to easily centralize and scale programs such as Virtual Nursing, Virtual Patient Observation, Virtual Rounding, and Virtual Consultations in inpatient settings, improving staffing flexibility and workflow efficiency and making it easier to engage remote specialists and interpreters to support patient access and health equity. Trusted by more than 1,000 U.S. hospitals for high reliability, the platform is favored for its adaptability to a multitude of workflows and integrations with clinical platforms, including Epic.
To learn more, contact Caregility at info@caregility.com.
About Baptist Health
For more than a century, Baptist Health has delivered all its best in health care through Christian compassion and innovative services. Baptist Health, Arkansas’s most comprehensive healthcare organization, is here For You. For Life. – with more than 250 points of access that include twelve hospitals, urgent care centers, a senior living community, over 100 primary and specialty care clinics, a college with studies in nursing and allied health, and a graduate residency program. It is also the largest private not-for-profit healthcare organization based in Arkansas, providing care through the support of approximately 11,000 employees, groundbreaking treatments, renowned physicians and community outreach programs. For more information about Baptist Health, visit Baptist-Health.com, call Baptist Health HealthLine at 1-888-BAPTIST or download the myBaptistHealth app.
About Caregility
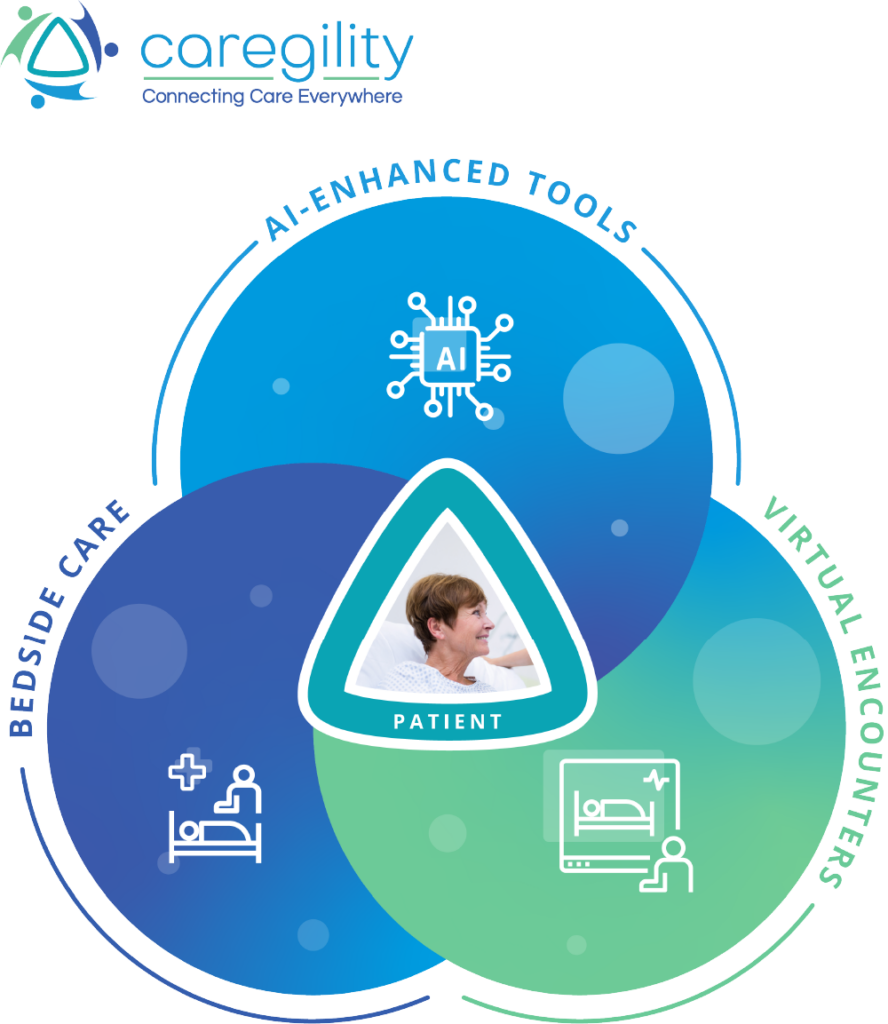
Caregility (caregility.com) is a telehealth solution provider connecting care everywhere. Designated as the Best in KLAS® Virtual Care Platform (non-EMR) in 2021, 2022, and 2023, Caregility Cloud™ brings bedside care, virtual encounters, and AI capabilities together at the point of care. Doctors, nurses, and patients around the world rely on our intelligent telehealth edge devices and virtual nursing, observation, and engagement applications to enhance clinical insights, patient safety, and efficiency. Trusted by over 75 health systems, deployed in more than 1,000 hospitals, and supporting over 30,000 connected devices and millions of virtual sessions annually, Caregility is helping transform healthcare delivery across inpatient, outpatient, and home settings.
Media Contact:
Jess Clifton
Senior Manager, Marketing Communications
jclifton@caregility.com
(678) 360-9043
HIMSS24 Takeaways: Healthcare’s New Table Stakes
In the wake of several challenging years for healthcare, health IT conference-goers showed up at the 2024 HIMSS exhibit with renewed enthusiasm and a discerning eye on ROI.
Attendees from healthcare institutions across the globe convened in Orlando, March 3-6, to explore solutions for “creating tomorrow’s health,” as the conference theme promised. The forum offered providers an opportunity to consider future-state possibilities and fresh approaches to persistent problems like process inefficiency and staffing challenges. AI and hybrid care solutions were on tap to answer both needs.
Responsible AI and the Hospital Room of the Future
In healthcare’s post-pandemic era, augmented intelligence and hybrid care models are bringing additional dimensions to the patient care team. The embrace of virtual care and AI at the patient bedside is redefining what we consider to be table stakes in care delivery.
Like the ViVE conference that drew healthcare stakeholders to the West Coast in the weeks prior, HIMSS24 showcased an overwhelming array of health AI innovations. As Caregility COO Mike Brandofino observed, you couldn’t walk the conference floor without bumping into an AI company.
During the conference, Brandofino sat down with HIMSS TV host Kate Milliken to dig into some of the ways health systems are using AI and hybrid care models to elevate the inpatient experience.
“The hospital room of the future is really about how you can use sensors in the room to augment information for the caregivers, thereby stretching what they can do,” said Brandofino.
“Our approach is what we call responsible AI. What we’ve done is focused on how we can enhance the information that’s getting to the caregiver. Things like vitals scanning – can we, just through an image of the patient’s face, get the blood pressure of the patient and give that to the clinician who is looking at the patient right now?”
Those solutions are closing care gaps, improving care quality for patients, and saving time for care teams. “We notify caregivers of changes that they need to pay attention to,” said Brandofino. “We don’t want to replace the caregivers. What we want to do is augment the information they have so they can spend more time maximizing their certification.”
Caregility’s “Intelligent Hospital Room of the Future” conference exhibit demonstrated ways health systems are using virtual collaboration, AI, and digital health integrations to build next-gen hybrid care models like radar-supported Virtual Nursing and computer vision-assisted Virtual Patient Observation.
A Hippocratic Oath for Health AI
Still, some providers are wary of adopting nascent technologies without proof of value and some reassurance.
As momentum builds for AI regulation on a national level, healthcare leaders are rising to meet the call for accountability within the medical field. During HIMSS24, Microsoft announced the creation of the Trustworthy & Responsible AI Network (TRAIN), “which aims to operationalize responsible AI principles to improve the quality, safety, and trustworthiness of AI in health.”
Fellow members of the TRAIN consortium include over a dozen leading health systems, OCHIN, and TruBridge. The group will share AI best practices, provide tools to enable the measurement of AI-related outcomes, and facilitate the development of “a federated national AI outcomes registry that will capture real-world outcomes related to efficacy, safety, and optimization of AI algorithms.”
As AI transparency initiatives unfold, the 2025 conference circuit could see a new system of checks and balances in place to help providers vet vendor offerings. For its part, HIMSS24 presented promising paths forward for providers keen on balancing innovation and ethics.
Caregility to Showcase the “Intelligent Hospital Room of the Future” at HIMSS24
EATONTOWN, NJ (March 7, 2024) – Caregility, a pioneer in enterprise telehealth solutions, is excited to showcase its Intelligent Hospital Room of the Future at the 2024 HIMSS Global Health Conference & Exhibition, taking place in Orlando, Florida, March 11-15. The installation, located at Caregility booth 4121, will highlight innovative technologies that are helping health systems transform clinical workflows to improve the care experience for patients and clinicians.
Built on the award-winning Caregility Cloud™ virtual care platform, the Intelligent Hospital Room of the Future brings together:
- AI-ready telehealth edge devices purpose-built for cost-effective, large-scale deployments that allow hospitals to leverage existing networks and in-room patient engagement platforms to extend virtual care and AI capabilities to every patient’s bedside.
- A self-healing telehealth platform with a proven track record of supporting millions of virtual care sessions annually that centralizes device fleet management and telehealth program and user administration.
- Intuitive care applications designed by clinicians for clinicians that streamline one-on-one and one-to-many workflows such as Virtual Nursing and Virtual Patient Observation.
- Responsible AI enhancements that augment patient safety, clinical insight, and operational value using computer vision, radar-based sensors, and sound analytics.
- Intelligent integrations with leading EHRs and nurse call systems, plus connected care devices like digital stethoscopes to share patient data with remote clinicians in real-time.
The Intelligent Hospital Room of the Future unlocks more efficient ways for care teams to field and standardize common tasks that can effectively be completed remotely, helping to offset staffing challenges and reduce stress on bedside clinicians. “Together, these solutions elevate the standard of care, improving patient satisfaction and creating a foundation for hybrid care model innovation,” said Caregility CEO Ron Gaboury.
As part of the exhibit, Caregility will demonstrate its first dual-camera telehealth edge device, the new APS200 Duo, for the first time. This intelligent telehealth endpoint includes AI-ready computer processing power, a wide-angle camera for patient observation, and a high-definition 40x zoom camera for supporting Virtual Nursing and other hybrid care programs such as Tele-ICU.
Visitors at booth 4121 can also explore integrated solution offerings from Caregility Cloud™ ecosystem partners, including virtual clinical services from Equum Medical and Hicuity Health, and interpreter services from LanguageLine Solutions. Attendees can also preview several integrated AI capabilities, including:
- Augmented Observation tools that help remote sitters keep at-risk patients safe, protect floor staff, and prevent disoriented patients from wandering.
- Vitals Trending tools that provide continuous, longitudinal insight into resting heart and respiratory rates to help care teams detect patient deterioration earlier and intervene faster.
- Vitals Scanning tools that use computer vision technology to remotely measure a patient’s blood pressure as well as heart and respiratory rates during virtual visits and exams.
HIMSS24 attendees are invited to tour the Intelligent Hospital Room of the Future at Caregility booth 4121 to learn more about how health systems are transforming the future of healthcare delivery through hybrid care enablement. Learn more at www.caregility.com/HIMSS-2024.
About Caregility
Caregility (caregility.com) is a telehealth solution provider connecting care everywhere. Designated as the Best in KLAS® Virtual Care Platform (non-EMR) in 2021, 2022, and 2023, Caregility Cloud™ brings bedside care, virtual encounters, and AI capabilities together at the point of care. Doctors, nurses, and patients around the world rely on our intelligent telehealth edge devices and virtual nursing, observation, and engagement applications to enhance clinical insights, patient safety, and efficiency. Trusted by over 75 health systems, deployed in more than 1,000 hospitals, and supporting over 30,000 connected devices and millions of virtual sessions annually, Caregility is helping to transform healthcare delivery across inpatient, outpatient, and home settings.
Caregility Media Contact:
Jess Clifton
Senior Manager, Marketing Communications
jclifton@caregility.com
(678) 360-9043
Hybrid Care in the Age of Retail Health
Amazon Clinics and other direct-to-consumer (DTC) healthcare market entrants are “disintermediating the traditional healthcare journey,” as Trilliant Health researcher Sanjula Jain, Ph.D., recently put it. As retail health options flood the field, patients are increasingly by-stepping PCPs in favor of DTC telehealth solutions to address their low-acuity healthcare needs.
- Amazon Clinic expands nationwide to provide messaging and video visits for common health conditions
- Walmart and Other Drug Stores Want to Help You Skip Trips to the Doctor
- Walgreens and VillageMD Expand Full-Service Primary Care Model to the Chicago Area
For those who can take advantage of DTC telehealth services, there is a clear convenience win. However, some argue that this disruption to the status quo is introducing additional fragmentation that can negatively impact patient care and provider operations.
Implications for Patients: One major question arising from the surge in retail care relates to the handling of patient data exchange. If a patient receives treatment from a retail health provider, how will that care episode be integrated into their primary health record?
Implications for Providers: For traditional healthcare providers, the rise of DTC healthcare models can result in a loss of critical patient insight or potential patient drift to other care delivery sources, eroding health system market share and revenue.
As we watch the debate over whether patients should also be regarded as consumers play out in a literal sense, here’s the reality: We are all patients seeking effective care and consumers demanding modern convenience and responsiveness. The ideal health system is one that delivers on both.
How Providers Can Compete
Competing in a modern healthcare market disrupted by retail health will require some degree of assimilation on behalf of healthcare provider organizations (HPOs). By establishing hybrid models of care that include virtual service offerings, providers can give patients the same easy access to low-acuity care as DTC alternatives, keeping patients within the health system.
Beyond creating clear and convenient pathways to non-urgent care, strategically wielding virtual care across the enterprise poses additional competitive benefits for health systems. When used at the bedside, inpatient virtual engagement tools introduce remote clinical support resources to patients and floor teams, improving patient experience and outcomes in mid-to-high acuity care encounters, as well. Integrated virtual care empowers HPOs to offset staffing challenges while keeping pace with other industries in terms of delivering the convenience and digital access consumers have come to expect.
With an aging patient population and chronic conditions on the rise, these tools will become even more essential to health systems’ survival. Looking ahead, HPOs can anticipate similar outside competition from retail health as Aging-in-Place and Hospital-at-Home programs continue to move the point of care beyond traditional brick-and-mortar institutions. Establishing the virtual care infrastructure now will help providers meet emerging demand by enabling remote monitoring and management of chronic conditions. Here, provider organizations that have the historic relationship and longitudinal patient data to support a more personalized care plan may garner an edge.
A Catalyst for Care Model Transformation
By embracing hybrid care, healthcare organizations can provide more convenient, personalized, and efficient care, which is crucial for competing against retail health competitors and meeting the evolving needs of the patient population.
Perhaps one of the reasons healthcare has historically lagged other industries in terms of innovation has been due to the absence of significant external threats. Whether this is true or not, it’s clear that healthcare as an industry is at an inflection point.
In a world rapidly moving towards direct-to-consumer health models, healthcare organizations can’t remain passive observers. To compete effectively, we must pivot, innovate, and integrate. By embracing hybrid care models, healthcare organizations can honor both the patient and consumer aspects of individuals and secure their place in the future landscape. The era of retail healthcare isn’t a threat; it’s an opportunity to evolve and provide better, more connected care everywhere.
Want to learn more about virtual care platform solutions for your health system? Set up a discovery call today!
AI-Enhanced Telehealth: Hope or Hype?
ChatGPT and a plethora of other AI-powered applications are rapidly gaining popularity in today’s tech-driven world. In healthcare, AI and machine learning algorithms are being adopted to drive efficiency in patient-facing and back-office settings alike.
One of the clinical frontiers gaining attention is the augmentation of virtual care programs with AI tools such as computer vision, ambient clinical intelligence, and contactless monitoring. By bringing these AI enhancements into virtual workflows in the inpatient setting, healthcare organizations hope to positively impact patient safety, clinical outcomes, care team experience, and operational performance.
During a recent fireside chat, Caregility President and COO Mike Brandofino sat down with Healthcare Innovation editor Mark Hagland to explore the practicality, best practices, and perils associated with selecting and adopting AI technology to advance telehealth.
AI’s Potential in Acute Virtual Encounters
AI is showing promise in clinical use cases in acute care settings where staffing shortages and burnout are prominent. As Brandofino sees it, one of AI’s biggest benefits is in “augmenting the information that a clinician or caregiver has access to with more clinical insight than they’d be able to gather on their own.” When evaluating tools, he encourages stakeholders to consider the impact: “Is it taking tasks away that can potentially save staff time? Is it a tool that adds to productivity?”
One of the AI functions Brandofino sees potential in is radar-based contactless monitoring. These tools continuously capture patient vitals such as heart rate and breathing rate, as well as track motion in the room. This allows caregivers to see trends over time.
“The AI part of that is the algorithms can detect changes in that pattern that mean something,” Brandofino explains. He offers a practical use case example. “That radar device can tell you, based on telemetry, that a patient is starting to wake up. Now think of a post-op situation where the nurses have to be there when the patient wakes up disoriented. Can you just have a contactless device notify them when the patient is starting to wake up so they can get in there then instead of sitting there for 30 minutes waiting?”
Automated, contactless vitals monitoring also accelerates the frequency and timeliness of clinical documentation.
“If you think about what happens with nurses as they do their rounds and take vital signs, many times they don’t get that information into the EHR until the end of their shift or hours later,” Brandofino notes. AI tools can gather vital signs many times throughout the day and put it through an algorithm to evaluate if the patient is getting better or worse. This allows care teams to intervene earlier and potentially improve outcomes.
Ambient clinical intelligence uses AI tools like natural language processing to draft clinical notes and reports, posing similar efficiency benefits. In care environments where resources are thin and burnout is high, those incremental time savings can add up.
Caveats to Consider When Adopting Health AI
As you evaluate AI solutions to bring into patient care delivery, it’s important not to become enamored with the technology before understanding where it fits into the patient care workflow. Brandofino recommends including all stakeholders—clinical, IT, and operations—in evaluations. “How are you going to support your device fleet? Consider the clinical workflow as well as the experience on the patient side.”
“Think about the operational logistics of supporting what you’re doing,” Brandofino advises. “What we suggest to our customers is to understand the impact that you’re going to have on the staff on the floor and think about what that is going to be like at scale.” Nurses are some of the most interrupted people in healthcare. The last thing you want to do is introduce new tools that add to their stress level, whether that be an overabundance of false alarms or device overload.
Given the newness of many AI tools entering the market, it’s also important to consider who you’re partnering with. Has the tool been implemented in one or two patient rooms or thousands of rooms? Are there examples of in-market success that can offer a roadmap?
Combining AI and Telehealth to Empower Caregivers
By integrating AI with virtual care, healthcare organizations can modernize care delivery with innovative new tools and keep the human element of care intact. AI can drive intelligent clinical alerting, while virtual engagement channels serve as a bridge for immediate staff intervention. When combined, these resources amplify what virtual teams are capable of supporting remotely, doubling down on reducing the burdens on bedside staff.
“We believe that combining that remote nurse with smart technology to help gather telemetry in the room will be really impactful in improving care for patients in the long term,” says Brandofino. “Don’t feel like you have to put in a siloed solution just to get access to AI technology. Look for players that are capable of integrating with what you already have. If you already have high-end cameras and mics in the room with edge processing, what else can you gather in the patient room to give to caregivers?”
Ultimately, healthcare organizations that focus on applying technologies that solve real problems that exist today around the shortage of nurses, productivity, and quality of life for staff will have the most impact.
Interested in learning more about AI-enhanced hybrid care solutions?
Contact us today!
Virtual Nursing Insights
Video
Virtual Nursing Insights
What if you could reduce clinician burnout, improve patient outcomes, and empower your team with new ways to deliver care? Virtual nursing, or tele-nursing, is creating a new path forward.
Virtual nursing addresses today’s chronic workforce challenges and sets your team up for future success as digital healthcare innovation redefines what care teams can accomplish remotely. Your nurses deserve it. And your patients depend on it.
Contact us to learn how we can help you build your virtual nursing program with our award-winning Caregility Cloud™ platform.
Inpatient Virtual Engagement for Hospital-Based Hybrid Care
Video
Inpatient Virtual Engagement for Hospital-Based Hybrid Care
To overcome workforce challenges and financial pressure, leading health systems are reimagining their telehealth strategy to bring virtual care into use cases at patient bedsides across the hospital enterprise.
Caregility’s Inpatient Virtual Engagement solutions are the first subscription-based offering for high-quality, cost-effective virtual care at scale – every room, every bed, every patient. Set up a discovery call with a member of our team to learn more!
Telehealth News Roundup: Virtual Nursing’s Rapid Rise
Buzz around virtual nursing is building. As telehealth sheds its COVID skin, the virtual care technology is entering a new phase of growth helping health systems advance acute care models to mitigate hospital workforce challenges.
In a recent interview with Commercial Integrator editor-in-chief Dan Ferrisi, Caregility President and COO Mike Brandofino addressed the rise of inpatient virtual care and, more specifically, virtual nursing.
“We lost a lot of nurses during COVID who retired, can no longer work, or just decided they didn’t want to [do it] anymore and we don’t have enough nurses coming in so there’s a huge shortage,” said Brandofino. “Virtual care is being used now to augment that.”
Nursing shortages during the pandemic led to labor cost inflation as hospitals battled for scarce resources. Recent CNBC coverage revealed that the “average pay for travel nurses was $150 an hour in early 2022, which analysts say tempted more nurses to leave staff jobs, increasing turnover and exacerbating shortages.”
That pay rate is three times higher than the national average for full-time staff nurses.
Virtual nursing offers health systems an alternative to expensive contract nurses that not only acts as a force multiplier for care teams but also enhances care collaboration and improves patient and clinician experience.
How Virtual Nursing Can Help Solve Many Workforce Shortage Woes
Healthcare IT News
Virtual care pioneer and Caregility Chief Nursing Officer Wendy Deibert, EMBA, BSN, RN, recently sat down with Healthcare IT News editor Bill Siwicki to offer a deep dive into the benefits of a hybrid approach to nursing that employs telehealth.
Virtual nursing programs are typically campus-based and staffed internally but can also be supported by third-party clinical services or a combination of the two. Workflows vary from campus to campus.
“Some organizations use virtual nurses for patient admissions and assessments or discharge education,” shared Deibert. “Others implement more comprehensive 24/7 patient surveillance and deterioration management programs. The fact that there is no one universal approach is really the beauty of telenursing. Programs can and should be tailored depending on your health system’s specific needs.”
Deibert noted that multiple organizations are actively working with stakeholders within the nursing community to develop virtual nurse certification programs to help establish standards for programs.
Virtual Nursing Programs Adapting to Organizational Needs
HealthTech Magazine
Meanwhile, organizations like Mary Washington Healthcare are forging their own path as early adopters of virtual nursing.
HealthTech Magazine editor Teta Alim highlighted the health system’s journey into virtual nursing in coverage of the 2023 American Telemedicine Association conference. Debra Marinari, Associate Vice President of Hospital Operations at Mary Washington Healthcare’s Stafford Hospital, and Heidi Steiner, MD, Clinical Program Manager at Caregility, were on site to share insight into the nursing workflows the hospital is working to virtualize, including admission assessment, plan of care, patient education, and discharge, to name a few.
Mary Washington Healthcare deployed an Inpatient Virtual Engagement solution to support its new virtual nursing program. According to Marinari, the leadership team will assess nurse engagement, patient satisfaction, the rate of nurse turnover, quality and safety metrics, and readmissions to measure program success.
Experts Weigh in on the Joys and Woes of Virtual Nursing
The Atlanta-Journal Constitution
Given the elevated rates of nurse attrition during and since the pandemic, many care teams are onboarding new hires who have limited field experience. As Atlanta Journal-Constitution writer Hunter Boyce shared, another benefit of virtual nursing is its ability to connect new nurses with experienced remote nurse resources who can help guide and mentor them. That secondary line of clinical reinforcement boots confidence for care team members, improving clinician experience and increasing the likelihood of retention.
As Walsh University nicely sums it up:
“The impact of technology on nursing practice cannot be overstated. When nursing technology takes over time-consuming routine processes, streamlining communication and delivering accurate diagnoses and personalized treatment plans, NPs are freed up to do the work that only humans can: providing one-on-one, compassionate care.”
Scaling Virtual Care
Programs like virtual nursing and continuous patient observation have rapidly risen to prominence as telehealth models mature on this side of the pandemic. The trend reflects an emerging hybrid care paradigm where remote and in-person engagement are blended to optimize patient care. Health systems can modernize care models and overcome many of the resource challenges hampering hospitals today by scaling virtual care to bring remote reinforcement into clinical workflows in acute settings and beyond.
To enable hybrid care across their enterprise, healthcare organizations are making virtual care and engagement accessible at every patient bedside. For many campuses, this means migrating away from siloed, pandemic-era telehealth implementations to a virtual care platform that’s better suited to support diverse clinical use cases.
As you’re scaling virtual care and refining your telehealth strategy, you want to establish infrastructure that is versatile enough to grow with you as needs change and your roadmap evolves. Here are five core tenets for ensuring long-term sustainability.
1) Reliable Infrastructure
Your virtual care platform is the heart of telehealth operations in your organization. Above all, you need a platform you can trust. Look for reliability across multiple areas, including HIPAA compliance and encryption security, ample capacity to support spikes in session concurrency, and uptime guarantees with retrospective analytics to back up claims. Conduct a network assessment with your solution partner early on to pinpoint and proactively address network weaknesses that may impede virtual care programs. Seek out partners who champion open communication and transparency in root cause analysis if and when issues arise.
2) User Experience
Ease of use can make or break adoption regardless of how much you invest in your virtual care platform. Solutions should avoid application download requirements for patient users and offer clinical users a consistent user experience across various workflows. Beyond the GUI, consider your experience with program builder, implementation, and IT support teams. Secure virtual care partners who are as easy to work with as the software and endpoint solutions they provide.
3) Centralized Administration
As operations expand, you’ll want a solution that allows you to easily manage your growing device fleet. Web-based administration portals help centralize managing multiple telehealth programs and allow remote governance and support of telehealth endpoints. Endpoint systems should be configured to proactively alert tech support remotely in case of malfunction and should be able to be restarted remotely. Reporting and analytics functionality should wield insight into program performance metrics and endpoint utilization.
4) Clinical Workflows
Clinically driven virtual care solutions that are purpose-built for specific workflows fare better than more generalized, one-size-fits-all solutions. Virtual care solution companies with extensive patient care experience on their bench bring clinical integrity to program development and can help bridge gaps between your internal IT and clinical teams. Both internal departments should be involved in strategy from the onset. Virtual clinical programs can and should be tailored to your health system’s specific needs. Start with one or two virtual workflows and expand from there.
5) Innovative Integrations
Virtual care platforms with API integration are ideal. They allow you to centralize core telehealth capacity while layering in integrations as you pilot emerging technologies. Each unit can tailor virtual care program workflows and resources for their unique needs. EHR integration allows clinicians to launch virtual sessions from a familiar work environment. Consider additional virtual care integrations such as clinical decision support (CDS), interpreter services, digital devices, and AI. Platforms that support HL7 and SMART on FHIR data standards help streamline interoperability and enable real-time access to patient data during virtual visits.
When scaling virtual care, it’s important to think multi-dimensionally about telehealth programs. What are your core workflow priorities? What additional resources can be brought into workflows to amplify efficiency and patient and clinician experience? Can programs be expanded to support multiple campus locations? By considering these variables early on you can develop a strategy that meets today’s challenges and sets the stage for continuous growth as hybrid care models continue to mature.
For a deeper dive into virtual care roadmapping and program implementation considerations, contact Caregility today to speak with one of our telehealth experts.







