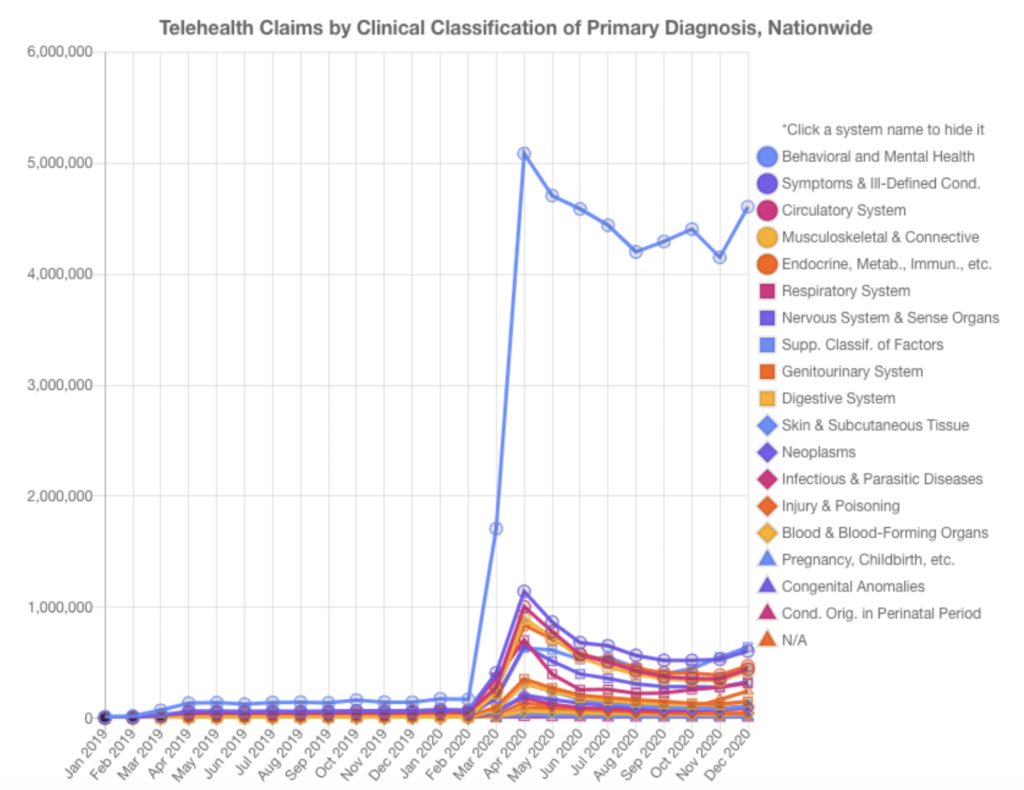
In April 2021, the COVID-19 Healthcare Coalition released an analysis of telehealth claims data to better understand the “dramatic shifts in the locus, roles, and reasons for seeking care during the pandemic.” The data the claims were derived from represented roughly 50% of all private insurance claims, de-identified, from January 1, 2019, through December 31, 2020.
What the coalition’s analysis showed is that telemedicine visits for behavioral and mental health practically dwarfed all other diagnoses:
As health systems continue to move past ad hoc telehealth implementations and look for enterprise telehealth solutions, it’s important that they understand the rising demand for behavioral health treatment, how technology can support that rising demand, and how telehealth can increase patients’ access to behavioral health providers.
Rising demand for behavioral health treatments
Demand for all kinds of telehealth rose during the pandemic—but demand for behavioral health truly skyrocketed. According to the claims analysis above, in the first month of the pandemic, telehealth visits for behavioral and mental health rose 1,000 percent. By the next month, the peak, they had risen nearly 3,000 percent, to more than 5 million.
Use has since tapered, but in the new year, all signs point to a sustained surge in demand for mental health services delivered via telehealth. A Kaiser Family Foundation survey showed that 4 in 10 adults reported symptoms of anxiety or depressive disorders during the pandemic. And, like in other specialties, those who delayed care during the pandemic are now seeking to have those concerns addressed.
Meanwhile, a separate KFF analysis showed that the geographic distribution of mental illness in the U.S. varies considerably across states:
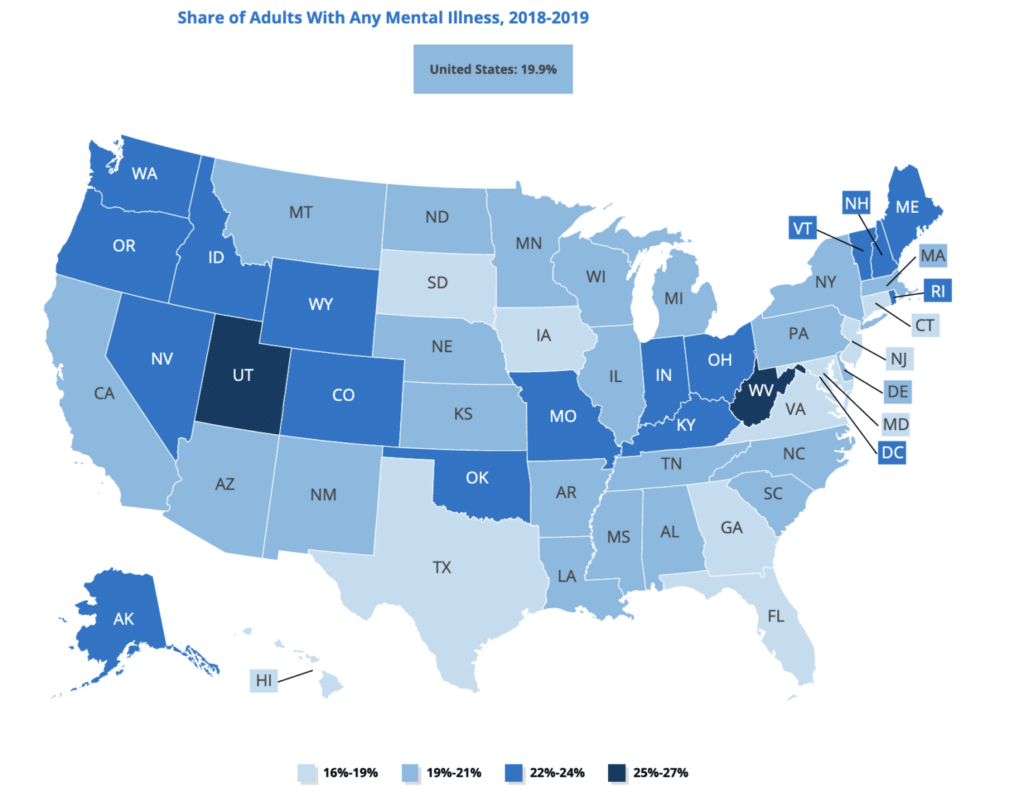
In Utah and West Virginia, for example, more than a fourth of adults reported some form of mental illness. States in New England, the Pacific Northwest, and scattered through the Midwest also reported higher rates of mental illness, while Texas, Florida, Georgia, Virginia, and Maryland, as well as Iowa and South Dakota, reported relatively lower incidences.
With demand rising, but also spread unevenly, telehealth is an increasingly relevant solution.
How technology can connect patients to telepsychiatry & behavioral health resources
The Commonwealth Fund categorizes the delivery of mental health into four models:
- Hub and Spoke. A familiar model for health systems, the hub and spoke centralizes specialists in one location, such as a hospital or large medical center, and uses telemedicine technology to connect to patients who visit outpatient clinics in the surrounding community.
- Integrated Care. In this model, primary care offices contract with a mental health provider or telemedicine technology solution to connect patients within that group practice to mental and behavioral health resources. Patients still access those resources at a clinical location.
- Direct to Consumer. Using telemedicine technology to go direct to consumers has truly exploded in recent months, with new investment flowing into the sector and stand-alone mental health services advertising direct to consumers, who can then access a mental health provider right from their home.
- Mobile Applications. These are similar to a Hospital at Home or remote patient monitoring program, but for mental health. In this model, patients use mobile technology to monitor their own symptoms and/or track prescribed mindfulness exercises designed to alleviate symptoms of depression or anxiety.
How telehealth options increase access to behavioral health providers
Providing remote access to behavioral health providers can dramatically improve access to care, especially for those in rural areas served by critical care access hospitals. In these locations, care providers often struggle to connect patients to the mental health resources they need.
Patients who come into the ER for a mental or behavioral health concern often need to be seen by a psychiatrist before the hospital can determine whether they should discharge them. In these cases, providing access to a psychiatrist via telehealth technology is a critical tool for hospitals to get the right care to behavioral health patients in a timely manner.
As the American Psychiatric Association reports: “There is substantial evidence of the effectiveness of telepsychiatry and research has found satisfaction to be high among patients, psychiatrists and other professionals.”
And, whereas prior to the pandemic state licensing requirements acted as a barrier to using telehealth to increase access across state lines, many of those requirements have since been dropped or temporarily waived. Now, all trends point toward safeguarding that access, especially for rural America.
Learn more about how Caregility’s telehealth technology platform can help support your organization’s mental or behavioral health program.







