A Turning Point for Rural Health: How States, Systems, and Digital Health Leaders Are Shaping What Comes Next
Rural America is in the middle of a rare and powerful moment of alignment. For decades, rural hospitals have been fighting a multidimensional battle: shrinking workforces, widening access deserts, aging populations with rising acuity, and tightening financial margins that make every operational decision existential.
This year, that burden meets an unprecedented opportunity.
Through the One Big Beautiful Bill Act, Congress authorized the $50 billion Rural Health Transformation Program (RHTP), a five-year infusion designed to help states rewrite the future of rural care delivery. States submitted their proposals to CMS in early November, and final funding decisions are expected by December 31, despite federal shutdown delays that required HHS to call furloughed reviewers back to keep things moving.
What happens next will determine whether this becomes a once-in-a-generation modernization of rural healthcare or another fleeting cycle of short-term relief.
Rural Health Needs are Urgent and Growing
Rural communities face higher rates of chronic disease, behavioral health needs, maternal health risks, and care access barriers. The workforce picture is equally stark:
- About 20% of the US population lives in rural areas, but only 9-11% of the nation’s physicians practice in rural communities. 1
- 74% of rural hospital CEOs report needing more RNs. 2
- RN staffing density is substantially lower in rural areas versus metro areas, with roughly 65 RNs versus about 100 RNs per 10,000 patients, respectively. 3
Some analyses suggest that a single transferred patient may represent a lost contribution margin of roughly $10,000, a financial reality that compounds the pressure to maintain local access.
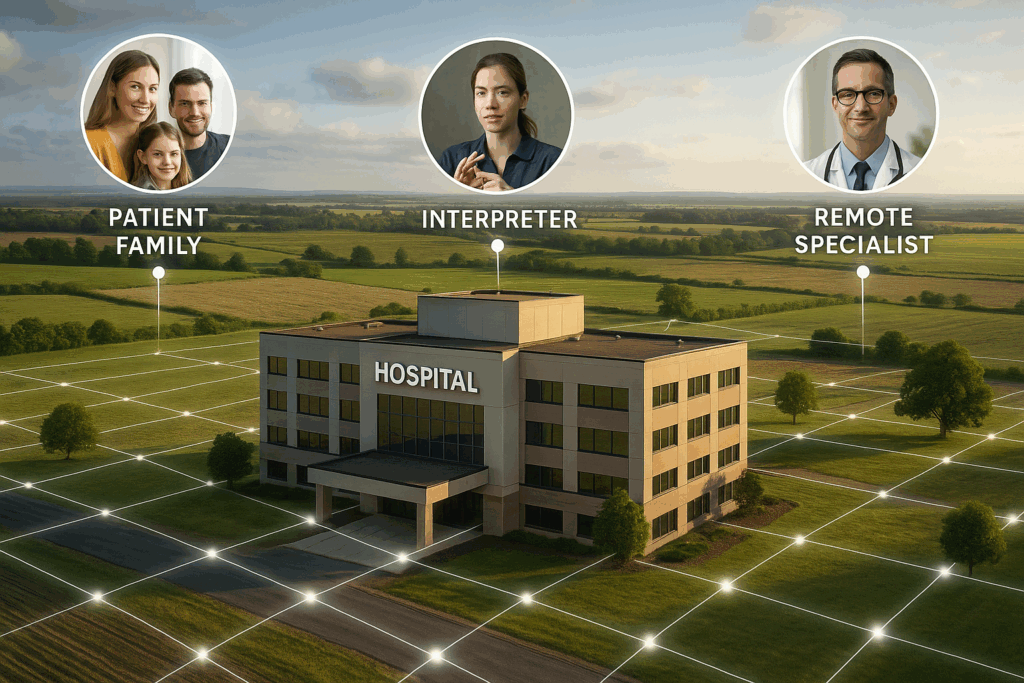
Against this backdrop, telehealth stands out as one of the most consistently emphasized modernization levers. In fact, “telehealth” appears 36 times in the RHTP framework, a signal that virtual care is essential to achieving the program’s goals.
Early Signals: How States Plan to Use Funding
Several states have already taken the lead in publicly sharing their RHTP applications, demonstrating an unusual level of transparency for a grant program of this scale. Details from early applications and announcements include:
- Maine proposes $200,942,115 over five years to expand telehealth access statewide. 4
- Washington plans to allocate $15–18 million annually toward a statewide Provider Technology Fund. 5
- Maryland, one of the first states to publish its proposal, emphasizes broad community engagement and technology-enabled care expansion. 6
These early examples show a common thread: states are prioritizing digital infrastructure, care innovation, and workforce sustainability, even though the strategies vary. In a review of 25+ state RHTP announcements, roughly 90% of states included telehealth hub or network language to advance specialist access through programs like tele-stroke, tele-ED, and tele-behavioral health. Workforce reinforcement and mobile telehealth access were also highlighted as key initiatives by many states.
Some may centralize funding through statewide contracts. Others will distribute funds through competitive grants, regional collaboratives, or direct sub-awards to rural facilities. This variation matters and hospitals that prepare early will have the most to gain.
What Rural Leaders Should Be Doing Right Now
During our recent National Rural Health Association (NRHA) webinar, four national thought leaders – Connor Communications Grant Strategist Angela Connor, MA; Caregility CNO Susan Kristiniak, DHA, MSN, RN, NEA-BC, AHN-BC; Health Recovery Solutions CEO Jason Comer, JD; and Equum Medical Chief Marketing Officer Karsten Russell-Wood, MBA, MPH – outlined a clear path forward for rural health organizations preparing for RHTP funding.
Here are the key themes they shared.
1. Prepare: Understand Your State’s Plan and Build Your Own
With RHTP approvals coming soon, Connor underscored the importance of early readiness, encouraging hospitals to:
- Review their state’s posted RHTP application to understand priorities, timelines, and distribution models.
- Contact their State Office of Rural Health, which will be central to coordinating sub-grants.
- Define strategic needs now, rather than waiting for a grant window to open.
- Build programs “as if budget weren’t the constraint,” to respond quickly and convincingly.
The takeaway: When states begin awarding funds, hospitals with clear, shovel-ready initiatives will be far ahead of those still brainstorming.
2. Repair: Rebuild Workforce Capacity with Connected Care Tools
Kristiniak brought the inpatient lens to the conversation: rural workforce strain isn’t theoretical. It shows up in fall rates, throughput challenges, safety risks, burnout, and rising overtime.
She emphasized how hybrid care models such as virtual nursing, virtual observation, remote specialist consults, and AI-enabled monitoring relieve both cognitive and physical burden on bedside teams. She highlighted data points rural hospitals can expect when leveraging virtual care:
- Faster admissions and discharges
- Reduced overtime
- Lower fall and hospital-acquired infection rates
- Shorter length of stay
- Better HCAHPS and discharge readiness scores
These are not abstract possibilities; they’re real outcomes already documented across community and rural hospitals using connected care models.
3. Care: Extend the Continuum Beyond the Hospital Walls
Comer spoke to the reality that modern rural care must extend beyond the inpatient setting. Longitudinal virtual care models such as Transitional Care Management, Remote Patient Monitoring, Chronic Care Management, and Advanced Primary Care Management are essential to the RHTP goals of keeping patients healthier, at home, and connected to their care teams.
He shared emerging success in areas like:
- Maternal health: early detection of cardiac complications and reduced postpartum risk
- Oncology: fever flagging, renal monitoring, and symptom tracking
- Cardiology and endocrinology: continuous, data-driven chronic condition management
These models are reimbursable, scalable, and aligned with RHTP’s emphasis on high-quality care as close to home as possible.
4. Solve the Specialist Gap with Fractional Coverage and Rural Networks
Russell-Wood highlighted a critical reality: many rural hospitals lose patients because they lose specialists. Recruitment cycles stretch 12 months or more, and locums can cost 1.5 to 2X the cost of a permanent hire.
Fractional models for specialties such as neurology, cardiology, pulmonology, and beyond allow hospitals to “subscribe” to the exact specialist time they need. Combined with regional telehealth collaboratives, this creates:
- Faster access to expertise
- Reduced unnecessary transfers
- Higher revenue retention
- Stronger local clinical confidence
These models directly support RHTP goals around sustainability, care access, and innovative delivery.
The Bigger Picture: Rural Health Is Entering a New Era
If there is a single takeaway from the NRHA panel, it’s this:
Rural hospitals cannot succeed in isolation. This is a moment for connected strategy, connected technology, and connected care.
For many rural leaders, this is the first time in their careers that strategic vision, federal investment, workforce innovation, and community need have aligned so clearly. The organizations that use RHTP funding to build durable, tech-enabled care models rather than one-off pilots will define what rural care looks like for the next decade.
Ready to Build Your RHTP-Aligned Roadmap?
Caregility partners with rural hospitals and state agencies to design sustainable virtual care programs aligned to the five strategic pillars of RHTP, from regional telehealth hubs to support specialist access to inpatient virtual nursing and AI-assisted observation.
If you’d like to explore how connected care can support your rural hospital’s transformation strategy, set up a discovery call today.







