Virtual Nursing FAQ
This resource draws from the expertise of Caregility Clinical Program Managers with decades of bedside nursing and virtual care implementation experience to addresses frequently asked questions about Virtual Nursing to support you on your adoption journey.
What is Virtual Nursing?

Virtual Nursing is a hybrid care model that involves using digital health technology to conduct targeted nursing tasks remotely to better support your bedside teams and enhance patient care.
Accessing the patient’s bedside using bidirectional telehealth, virtual nurses help assess, educate, and monitor patients throughout their inpatient care journey. Virtual nurses take on tasks that don’t require hands-on care, so floor nurses are free to focus on more complex patient encounters.
What are the benefits of Virtual Nursing?

Virtual Nursing helps your healthcare organization mitigate nurse burnout, improve patient satisfaction, and increase clinical team efficiency by redistributing patient care tasks to remote nurses. This gives valuable time back to bedside nurses, supporting nurse retention. The uninterrupted nature of standardized Virtual Nursing workflows also reduces the time it takes to complete tasks, resulting in improved patient throughput. Patients and staff alike benefit from a secondary line of clinical support at the bedside.
What are common obstacles when launching Virtual Nursing programs?
Common challenges to Virtual Nursing implementation include:
Infrastructure Readiness: Ensuring the necessary physical infrastructure is in place to support smart technology in every patient room can be a hurdle. Your data and network connectivity may need to be enhanced, particularly in older facilities, which can be challenging when rooms are in use.
Network and Security Protocol: Traditional network and security management approaches such as forced logouts, device timeouts, firewall port restrictions, IP address reassignments, Wi-Fi over-subscription, and bandwidth restrictions, warrant reassessment to ensure security without clinical disruption in care environments where devices must be available 24/7.
Nurse Buy-In: Gaining the support of your bedside nurses is crucial, as their hesitance can impede implementation. Streamlining communication between clinical and technical teams as well as virtual and bedside nursing teams is essential for smooth operations. Finding time for clinical teams to try new tech is another challenge to overcome, particularly as staffing challenges continue to put pressure on care teams.
How can healthcare organizations get started with Virtual Nursing?
 Virtual Nursing programs may look quite different across organizations, depending on your needs, resources, and infrastructure. Here are some of the key decision points that will ultimately determine what Virtual Nursing looks like for your healthcare organization.
Virtual Nursing programs may look quite different across organizations, depending on your needs, resources, and infrastructure. Here are some of the key decision points that will ultimately determine what Virtual Nursing looks like for your healthcare organization.
Define Your Goals: Identify performance areas you would like to improve, such as reducing nurse burnout and overtime or improving patient outcomes, to help inform your program use cases.
Identify Initial Workflows: Select clinical workflows that Virtual Nursing can enhance, focusing on tasks with the highest impact on your targeted performance improvement areas.
Evaluate Technical Needs and Infrastructure Readiness: Collaborate with IT to scope out your technical needs and ensure your network can support the unique nature of always-on virtual care.
Settle on a Staffing Model: Determine if virtual nursing staff will be insourced or outsourced, where insourced talent will work from, and what your virtual nurse-to-patient ratios will look like.
Implement Enabling Technology: Determine if mobile telehealth carts, mounted telehealth devices, or a tablet-based strategy will best support your program and identify key integration needs.
Establish a Process to Quantify Performance: Benchmark nursing performance measures pre-implementation to act as a threshold to compare your Virtual Nursing program outcomes against.
Pilot Your Initial Workflows: Work with bedside and virtual nurse teams to routinely gather feedback on program performance to optimize processes.
Scale to Additional Workflows and Units: Building on what you learn from your pilot, develop a plan to extend Virtual Nursing wins in additional units and workflows.
Where can healthcare organizations deploy virtual nurses?
Virtual Nursing has broad applicability. Beyond its use within general Med/Surg units, virtual nurses can reinforce patient safety initiatives like virtual sitting, ED triage, and early sepsis detection, as well as support specialty care like Cardiology, Neurology, and Oncology. Virtual nurses can also be used to support workflows in outpatient settings as well as home-based care programs.
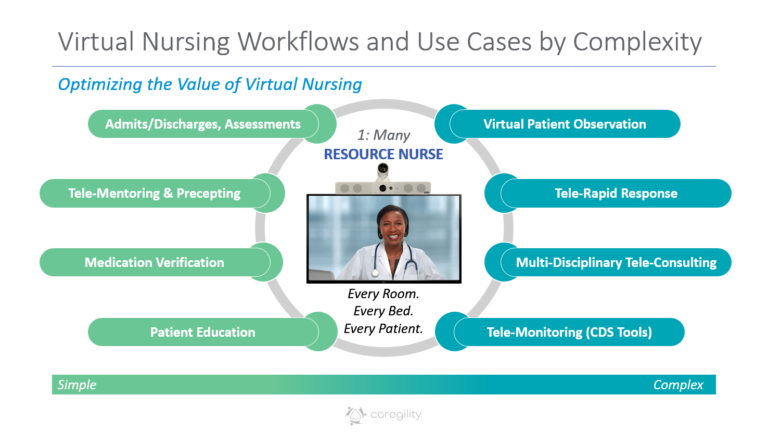
What are the most common Virtual Nursing workflows that healthcare organizations pursue?
Admissions, discharges, and patient education are among the most common workflows health systems adopt to get started. Additional simple Virtual Nursing workflows include tele-mentoring and precepting for new staff, multidisciplinary rounding, and deterioration monitoring.
What are some of the more complex workflows or use cases for Virtual Nursing?
Virtual patient observation or virtual sitting, tele-rapid response, blood and medication verification, specialty consult coordination, and more advanced tele-monitoring with Clinical Decision Support represent some of the more complex use cases for Virtual Nursing.
What staffing models and ratios are commonly used in Virtual Nursing?
Staffing models for Virtual Nursing vary across organizations and may include:
Dedicated Virtual Nursing Departments: Health systems may create specialized teams for Virtual Nursing and other hybrid care programs that work from a designated location within the healthcare organization.
Rotational Models: Many health systems elect to rotate virtual nursing shifts from traditional bedside teams so that nurse familiarity is already established and care teams can focus on process optimization.
Outsourced Clinical Support: For health systems in rural and underserved areas with limited nursing pools to draw from, outsourced clinical services offer a viable alternative to travel nurses.
Virtual nurse-to-patient ratios vary depending on the scope of the program, but the majority of Caregility customers’ early pilots have ranged from ten to thirty patients per virtual nurse. Most commonly, care teams look to the average number of expected admissions and discharges by shift to help establish initial ratios, with higher levels of remote staff available during busiest hours.
What are favorable characteristics to look for in a virtual nurse?

Tenured nurses with extensive bedside experience are ideal candidates for virtual nursing. Virtual nurses should be assertive yet personable, good at multi-tasking, and comfortable with technology. They should also be good problem-solvers with high emotional intelligence who are adept at picking up on nonverbal cues.
Bedside nurses who are burned out, seeking a change, or considering retirement are also good candidates for virtual nursing roles. This helps to preserve valuable institutional knowledge for the organization and supports career extension for seasoned nurses.
How do you garner buy-in and involvement from bedside nurses?
Involving bedside nurses from the outset is essential for the successful implementation of Virtual Nursing. Engage bedside nurses in the planning and design of Virtual Nursing workflows to align solutions with their needs and pain points. Capture continuous feedback through staff surveys and daily huddles to maintain open lines of communication that support workflow improvements.
How do you build collaboration between bedside and virtual nurses?
Building a strong rapport between bedside and virtual nurses is crucial for a collaborative environment. This can be achieved through joint training sessions designed to help both sets of nurses understand their respective roles and how they complement each other. When possible, occasionally rotating the roles between bedside and virtual nurses can foster mutual respect and understanding, promoting teamwork.
What are best practices for determining Virtual Nursing ROI?
To measure the return on investment (ROI) for Virtual Nursing programs, consider these approaches:
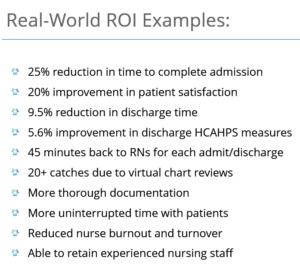
Time Studies: Conduct detailed time study analyses for various workflows, comparing pre- and post-implementation performance averages to quantify time savings achieved by virtualizing tasks. Workflow efficiency gains can reduce staff overtime and accelerate bed turnover.
Patient and Staff Surveys: Use patient and staff experience surveys to gauge satisfaction levels and identify areas for improvement. Many health systems see hard and soft ROI due to improved patient experience as reflected in HCAHPS scores due to the uninterrupted nature of virtual nurse engagement. Health systems also see ROI in reduced staff burnout and improved nurse retention.
Clinical Quality Metrics: Benchmark pre-implementation performance indicators – i.e., patient falls, length of stay, etc. – to weigh against clinical performance post-implementation. Cost avoidance due to earlier intervention is one of the strongest points of Virtual Nursing ROI.
What technical considerations should healthcare organizations be aware of when implementing Virtual Nursing?
Security, high reliability, and the ability to field workflows from within your organization’s EHR are table stakes for an effective Virtual Nursing program. You’ll also want to consider workstation requirements for your Virtual Nursing teams.
There are a few strategies your organization can take regarding bedside telehealth enablement:
Mobile Devices: Many healthcare organizations initiate Virtual Nursing pilot programs using a Bring-Your-Own-Device strategy that employs smartphones or tablets at the patient bedside to keep initial costs down.
Mobile Telehealth Carts: Health systems also frequently repurpose mobile carts used to support programs like Virtual Sitting to enable Virtual Nursing. This offers flexibility to extend virtual care support to wherever it’s needed, using technology the team is already familiar with.
Mounted Telehealth Edge Devices: As Caregility customers move from pilots to widescale program adoption, many are moving to adaptive telehealth devices that integrate with smart TVs and Interactive Patient Consoles in the patient room to create a consolidated virtual engagement hub at each bedside. Dual-camera edge telehealth devices enable care teams to support multiple virtual workflows, from one-on-one patient engagement to one-to-many virtual patient observation, as well as emerging clinical AI capabilities.
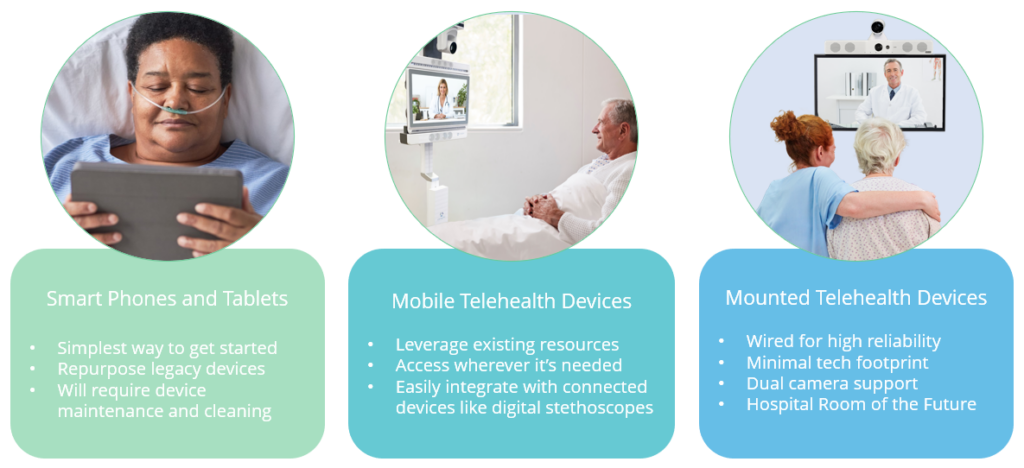
An important aspect of Virtual Nursing enablement is centralized device fleet management. Identify a virtual care platform that can support devices and workflows across your organization to standardize the experience and scale more easily over time.
What technology integrations are essential for Virtual Nursing?
Beyond EHR integration, common adjacent technologies for Virtual Nursing include:
- Clinical Decision Support (CDS) systems that provide virtual nurses with real-time insights to make informed decisions
- Connected medical devices like digital stethoscopes to facilitate remote patient monitoring (RPM)
- Interactive Patient Consoles (IPCs) in the patient room to minimize IT redundancies
- Interpreter services to support health equity and language access for deaf and limited-English-proficient patients
- Nurse call systems to streamline clinical notification and response
- Outsourced clinical services to help fill virtual nurse roles as needed
Does AI play a role in Virtual Nursing?
Yes, artificial intelligence (AI) has significant potential to enhance Virtual Nursing by enriching the patient information that nurses have access to. Clinical AI use cases include:
Augmented Observation: Use computer vision-based AI to track clinician, patient, and visitor activity in the patient room for an added layer of security for patient and staff safety.
Vitals Scanning: Use transdermal optical imaging AI to remotely assess patient blood pressure and heart and respiratory rates with a 30-second scan during virtual visits.
Vitals Trending: Use radar-based AI for contactless, continuous monitoring of patient heart and respiratory rates to support early detection of decline, alerting the nurse if rates trend out of range.
Additional Resources